Most people with mild-to-moderate COVID-19 produce antibodies that can fight off the infection that remain at similar levels in the body for at least 5 months, suggests research carried out at Icahn School of Medicine at Mount Sinai in New York.
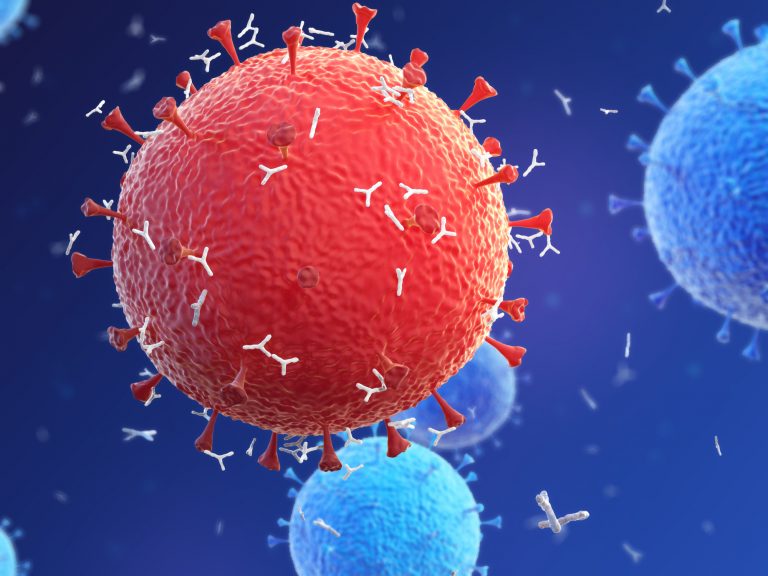
Although the researchers caution that further work is needed to confirm how much these antibodies protect people from re-infection, they found that the antibodies produced were able to neutralize SARS-CoV-2 suggesting that they have a protective role.
“While some reports have come out saying antibodies to this virus go away quickly, we have found just the opposite – that more than 90% of people who were mildly or moderately ill produce an antibody response strong enough to neutralize the virus, and the response is maintained for many months,” said Florian Krammer, Ph.D., a professor at the Icahn School of Medicine at Mount Sinai and a senior author of the paper about the research, which is published in the journal Science.
Krammer and team screened 30,082 people with mild-to-moderate infections who were tested at Mount Sinai Health System in New York City. The individuals included in this study were recruited as part of a screening drive that started in March to recruit donors of antibody-positive plasma. The team used a highly specific (100%) and sensitive (92.5%) enzyme-linked immunosorbent assay designed to detect antibodies targeting the SARS-CoV-2 spike protein.
Of those in the cohort, only 7.1% had an antibody level that was considered to be ‘low’ (1:160 or lower). Of those that remained, 22.5% had a ‘moderate’ level (1:320) and 70.4% a ‘high’ level (1:960 or higher).
To assess how these antibody levels persisted over time, the researchers randomly selected 121 participants in the cohort to follow-up with a range of initial antibody levels. This group were retested an average of 82 days and 148 days after their initial measurements were taken. Although antibody levels had declined a small amount, they were still at least at a moderate level, even 5 months after initial testing, in most people.
Some people with initially low levels of antibodies, actually had an increase in levels at 82 days, but these had dropped back to initial levels or lower by 148 days, which the researchers say corresponds to previous reports that people with mild infections can take longer to mount a full antibody response.
“Uncovering the robustness of the antibody response to SARS-CoV-2, including its longevity and neutralizing effects, is critically important to enabling us to effectively monitor seroprevalence in communities and to determining the duration and levels of antibody that protect us from reinfection. This is essential for effective vaccine development,” commented Krammer.
The authors note that as most IgG antibodies decline to 50% of their initial levels in only 21 days, the sustained levels seen in this group are probably being produced by long-lived plasma cells in the bone marrow.
“The serum antibody titer we measured in individuals initially were likely produced by plasmablasts, cells that act as first responders to an invading virus and come together to produce initial bouts of antibodies whose strength soon wanes,” explained Ania Wajnberg, M.D., Director of Clinical Antibody Testing at the Mount Sinai Hospital and first author of the paper.
The researchers plan to continue to follow-up individuals in this cohort to assess how their antibody levels change over time. They will also investigate further how protective these antibodies are against re-infection with SARS-CoV-2.













