A multidisciplinary research team at Harvard’s Wyss Institute for Biologically Inspired Engineering has developed a microfluidic organ chip the size of a USB memory stick that recapitulates key pathological hallmarks from CF patients more accurately than other current in vitro systems. The model replicates CF-specific changes in multiple hallmarks of the disease, including in the airway’s mucus layer, the beating of mucus-transporting cilia, pathogen growth, inflammatory molecules, and the recruitment of white blood cells, providing a comprehensive preclinical human model in which to investigate new CF therapies. Findings from the new study were published recently in the Journal of Cystic Fibrosis.
“Now that we are able to accurately model CF pathology, including microbiome and inflammatory responses, in human Airway Chips, we have a way to attack challenges that are important to CF patients,” explained senior study author Donald Ingber, MD, PhD, founding director at the Wyss Institute. “The bundled capabilities of this advanced in vitro model can help accelerate the search for drugs that may dampen the exaggerated immune response in patients, treat them with more personalized therapies and, help solve problems that CF patients face every day which cannot be addressed by existing treatments.”
To model and compare the microstructure and function of vascularized CF airways, the authors grew lung airway cells obtained from human CF patients or healthy individuals in one of two parallel running hollow channels of a microfluidic device under air, recapitulating the lung’s air-transporting environment. In the second channel, which is separated from the first one by a porous membrane, they recreated a human blood vessel from human lung microvascular cells that were perfused with a blood substitute medium.
“This first microphysiological model of a CF airway closely mimics what we know from airways in CF patients. Maintaining the typical composition of all relevant cell types, it developed a thicker mucus layer, and its ciliated cells exhibit higher densities of cilia that beat at a higher frequency compared to Airway Chips created with airway cells from healthy individuals,” said co-first author and a former postdoctoral fellow on Ingber’s team, Ratnakar Potla, PhD. “Importantly, these pathological changes were accompanied by an enhanced inflammatory response in the modeled CF bronchial epithelium that is much like the one observed in CF patients.” Potla is now a senior scientist of the complex in vitrosystems at Genentech-Roche.
After culturing the Airway Chips for two weeks, the researchers measured the levels of pro-and anti-inflammatory factors flowing out of the Airway Chip’s vascular channel that are known to be involved in the inflammatory response in the lungs of CF patients. Among other changes, the level of the pro-inflammatory cytokine IL-8 was increased in CF chips compared to those in control Airway Chips. Interestingly, IL-8 is known for its ability to attract the type of white blood cells known as neutrophils that also drive inflammation in the lungs of CF patients.
When the researchers then actually flowed human neutrophils through the vascular channel of the CF Airway Chips, they observed that more of the immune cells spontaneously adhered to the surface of vascular cells, squeezed themselves through the vascular cell layer and porous membrane, and accumulated in the airway epithelial cell layer of the air channel—recapitulating a process known as “transmigration.”
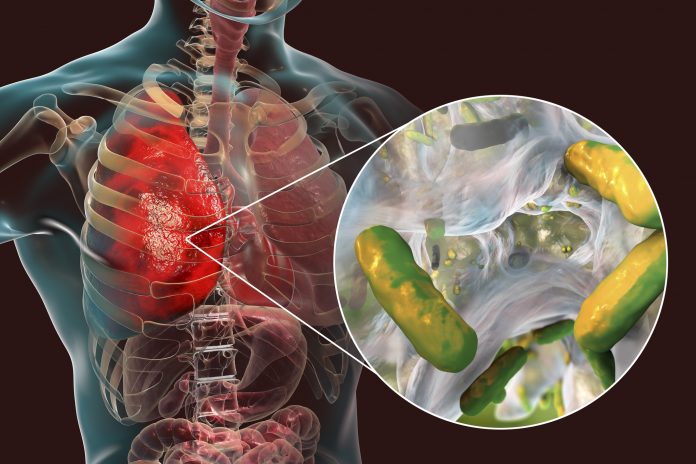
But the CF-mimicking airway tissue not only stimulated immune cell recruitment, but it also supported the growth of the bacterium, Pseudomonas aeruginosa, which is present in the microbiome of the normal lungs but can grow out of control and cause lung infections in human CF patients. Twenty-four hours after they introduced a fluorescently labeled version of P. aeruginosa into the airway channel of chips created with bronchial epithelial cells from CF patients, the team detected higher numbers of the pathogen in CF-specific mucus than in mucus in healthy Airway Chips. As a consequence, the levels of pro-inflammatory cytokines were further increased, thus replicating the infection-inflammation cycle seen in CF patients.
As the next steps, the team will further personalize their CF Lung Airway Chip by generating versions in which bronchial epithelial, vascular endothelial, and immune cells are obtained from the same patient. “For this proof-of-concept study, we have only used CF-specific bronchial airway cells from patients carrying the frequent ΔF508 CFTR mutation. But different CFTR mutations may also affect the function of endothelial and immune cells and differ in their effects,” concluded co-first author Roberto Plebani, PhD, a visiting professor from the University of Chieti-Pescara in Italy. “By developing a panel of patient-specific Airway Chips using cells from patients with different mutations, and also by directly measuring the activity of differently compromised CFTR ion channels on-chip, drug responses, and efficacies could be investigated in a highly personalized manner.”











