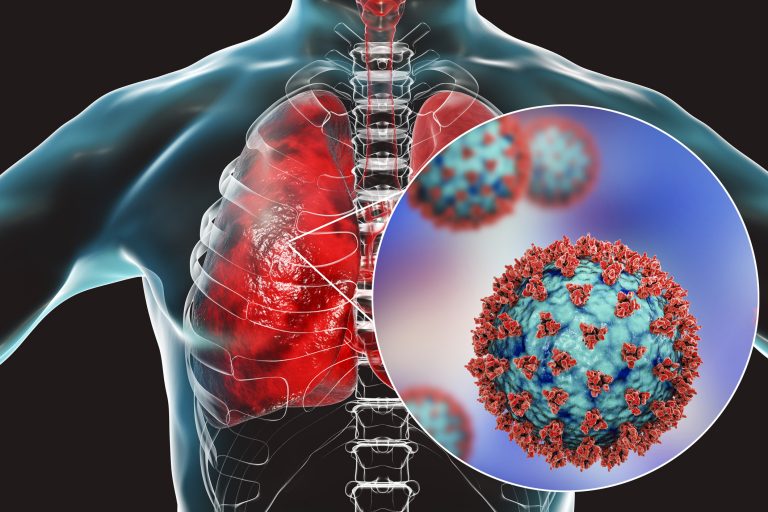
White blood cells called neutrophils have already been implicated in severe COVID-19 by studies linking SARS-CoV-2-associated lung pathology and large numbers of circulating neutrophils. Although neutrophils cast sticky, microbe-fouling neutrophil extracellular traps (NETs) made of DNA, they can be overzealous, damaging the body’s own tissues. Additional support—large numbers of NETS distributed throughout the lungs, and elevated numbers of NETs in plasma—comes from two studies that appeared September 14 in the Journal of Experimental Medicine (JEM).
The first study, “Neutrophil extracellular traps infiltrate the lung airway, interstitial, and vascular compartments in severe COVID-19,” comes from Liege University, where researchers led by Thomas Marichal, Cécile Oury, and Philippe Delvenne found substantial quantities of NETs in distinct compartments of the lungs of patients who died from COVID-19 and who exhibited histopathological features of diffuse alveolar damage. In contrast, noted Marichal, the NETS “were absent in the lungs of patients who died from another cause.”
According to the researchers, NETs NETs were also formed at sites of inflammation located in the interstitial compartment between the alveoli and blood vessels, and could even be seen in the blood vessels themselves near tiny blood clots known as microthrombi.
“NETs were found in the airway compartment and neutrophil-rich inflammatory areas of the interstitium, while NET-prone primed neutrophils were present in arteriolar microthrombi,” Marichal and colleagues wrote in JEM. “Our results support the hypothesis that NETs may represent drivers of severe pulmonary complications of COVID-19 and suggest that NET-targeting approaches could be considered for the treatment of uncontrolled tissue-damaging and thrombotic responses in COVID-19.”
“NETs can form a platform for the adhesion of platelets and other blood-clotting factors,” he explained. He added, however, that whether NETs actually contribute to the formation of COVID-19-associated pulmonary microthrombi will require further investigation.
In the second study, “SARS-CoV-2–triggered neutrophil extracellular traps mediate COVID-19 pathology,” a team of researchers led by Fernando Queiroz Cunha, Flavio Protasio Veras, and Thiago Mattar Cunha at the University of São Paulo also identified increased numbers of NETs in the lungs of severe COVID-19 patients and found that NET formation was elevated in COVID-19 patients’ blood plasma as well.
“We found that viable SARS-CoV-2 can directly induce the release of NETs by healthy neutrophils,” the researchers emphasized. “Mechanistically, NETs triggered by SARS-CoV-2 depend on angiotensin-converting enzyme 2, serine protease, virus replication, and PAD-4.”
Finally, NETs released from SARS-CoV-2-infected neutrophils were seen to induce the death of lung cells grown in the lab. However, the researchers found that cell death can be prevented if NET release is inhibited or the NETs are degraded by an enzyme that chews up DNA.
“Our study,” said Cunha, supports the use of inhibitors of NET synthesis or promoters of NET fragmentation as a strategy to ameliorate the organ damage associated with severe COVID-19.”













